Have you ever woken up in the middle of the night with a sharp, stabbing pain in your stomach? Or perhaps you’ve experienced a dull ache that lingers throughout the day? Abdominal pain is a common complaint that can range from mild and fleeting to severe and debilitating. Its causes are vast, spanning from simple indigestion to serious medical conditions. Navigating this discomfort can be a daunting experience, especially when you’re unsure of its root cause. This is where a nursing care plan comes into play, providing a roadmap for understanding, treating, and managing abdominal pain.
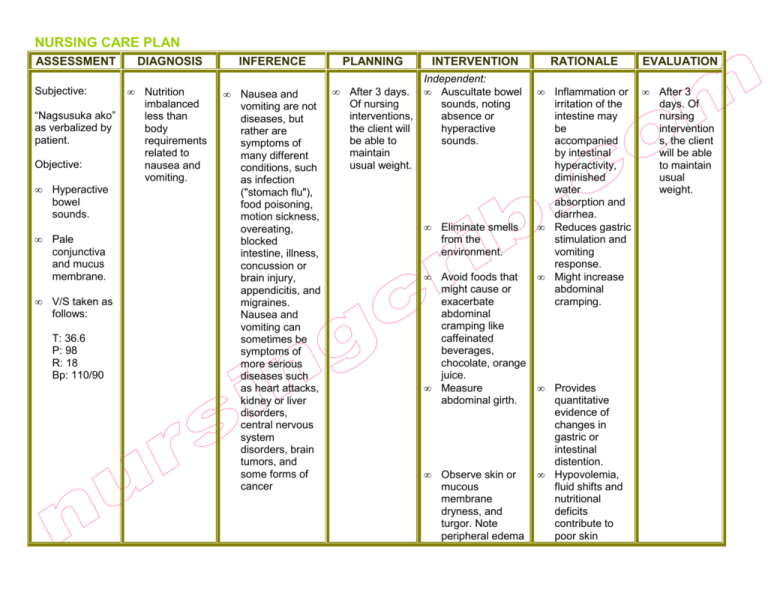
Image: studylib.net
In this comprehensive guide, we’ll delve into the intricacies of a nursing care plan for abdominal pain. We’ll explore the steps involved in assessing the situation, identifying potential causes, and implementing interventions to alleviate discomfort. By understanding the principles behind this plan, you can empower yourself with valuable knowledge and navigate this challenging journey with greater confidence.
Understanding the Scope of Abdominal Pain
The human abdomen houses a complex network of organs, including the stomach, intestines, liver, gallbladder, pancreas, and kidneys. Any disruption in these organs can trigger pain, making its causes incredibly diverse. Here’s a breakdown of the major categories:
1. Gastrointestinal Issues:
- Indigestion: This common discomfort stems from difficulty digesting food, often caused by overeating, fatty foods, or certain beverages. It can manifest as a burning sensation in the chest, bloating, and a feeling of fullness.
- Gastroesophageal Reflux Disease (GERD): When stomach acid flows back into the esophagus, it can cause heartburn, chest pain, and a sour taste in the mouth.
- Irritable Bowel Syndrome (IBS): This chronic disorder affects the large intestine, leading to abdominal cramps, bloating, diarrhea, and constipation.
- Appendicitis: Inflammation of the appendix, a small pouch attached to the colon, can cause severe pain in the lower right abdomen, nausea, vomiting, and fever.
2. Inflammatory Conditions:
- Peritonitis: Inflammation of the peritoneum, a membrane lining the abdominal cavity, can occur due to infections or injuries, causing severe abdominal pain, fever, and tenderness.
- Pancreatitis: Inflammation of the pancreas can cause intense abdominal pain, often radiating to the back, nausea, vomiting, and fever.
3. Other Causes:
- Kidney Stones: These hard deposits in the kidneys can cause intense pain radiating to the abdomen, flank, and groin, along with nausea, vomiting, and blood in the urine.
- Pelvic Inflammatory Disease (PID): Infection of the reproductive organs can cause lower abdominal pain, pelvic pain, fever, and abnormal vaginal discharge.
- Endometriosis: A condition where uterine tissue grows outside the uterus can cause pelvic pain and menstrual irregularities.
- Ectopic Pregnancy: When a fertilized egg implants outside the uterus, it can cause severe abdominal pain, pelvic pain, vaginal bleeding, and potential life-threatening complications.
- Constipation: This common digestive issue can cause abdominal pain, bloating, and difficulty passing stools.
- Food Poisoning: Ingesting contaminated food can cause abdominal pain, nausea, vomiting, diarrhea, and fever.
- Peptic Ulcer Disease: Open sores in the lining of the stomach or duodenum can cause severe pain, typically after eating.
A Holistic Approach: The Nursing Care Plan for Abdominal Pain
A comprehensive nursing care plan goes beyond simply alleviating pain. It aims to identify the underlying cause, provide supportive care, educate the individual, and collaborate with other healthcare professionals. Here’s a breakdown of the essential components:
1. Assessment:
- History Taking: The nurse gathers information about the pain’s onset, location, duration, character (sharp, dull, cramping), aggravating and relieving factors, associated symptoms (nausea, vomiting, diarrhea, fever), and past medical history.
- Physical Examination: The nurse observes the individual’s appearance, vital signs (temperature, pulse, respiration, blood pressure), and performs an abdominal assessment, including inspection, palpation, percussion, and auscultation.
- Diagnostic Tests: Depending on the suspected cause, the nurse may recommend laboratory tests (blood count, urine tests, stool analysis), imaging studies (X-rays, ultrasound, CT scan, MRI), or endoscopy (gastroscopy, colonoscopy).
2. Nursing Diagnoses:
Based on the assessment, the nurse identifies potential nursing diagnoses, which describe the individual’s health challenges. Examples include:
- Acute Pain: The individual experiences severe pain that requires immediate attention.
- Impaired Gas Exchange: The individual experiences breathing difficulties related to abdominal pain.
- Risk for Deficient Fluid Volume: The individual may be at risk for dehydration, especially if experiencing vomiting or diarrhea.
- Anxiety: The individual may experience anxiety and fear related to the pain and uncertainty of its cause.
3. Planning:
The nurse develops a personalized care plan that includes measurable goals and specific interventions. Goals might include:
- Pain Relief: Reducing the severity and frequency of pain to a manageable level.
- Improved Gas Exchange: Maintaining normal respiratory function.
- Adequate Hydration: Ensuring adequate fluid intake to prevent dehydration.
- Reduced Anxiety: Reducing anxiety and promoting a sense of calm.
4. Implementation:
The nurse provides various interventions, tailored to the individual’s needs, which may include:
- Pharmacological Interventions: Pain medication, anti-nausea medications, antidiarrheal agents, or antibiotics may be prescribed.
- Non-Pharmacological Interventions: Warm compresses, relaxation techniques, guided imagery, and deep breathing exercises can help manage pain and reduce anxiety.
- Nutritional Interventions: A bland diet, avoiding spicy or fatty foods, may be recommended to reduce digestive stress.
- Fluid Management: Adequate hydration is crucial, especially if experiencing vomiting or diarrhea.
5. Evaluation:
The nurse regularly evaluates the effectiveness of the care plan by monitoring the individual’s pain levels, vital signs, response to interventions, and overall well-being. Adjustments to the plan may be made based on the individual’s progress.
Navigating Pain: Practical Tips for Self-Care
While medical intervention is often necessary, there are steps you can take to manage abdominal pain at home. Remember, it’s crucial to consult a healthcare professional if the pain is severe, persistent, or accompanied by other alarming symptoms. Here are some helpful tips:
- Stay Hydrated: Drink plenty of water, clear broth, or sports drinks to prevent dehydration.
- Rest: Getting sufficient rest can allow your body to heal and reduce strain on the digestive system.
- Dietary Changes: Avoid trigger foods that exacerbate your symptoms, such as spicy, greasy, or acidic foods.
- Over-the-Counter Pain Relief: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen can provide temporary pain relief. However, use them cautiously and consult your doctor about suitable dosages.
- Warm Compresses: Applying a warm compress to the abdomen can help relax muscles and relieve pain.
- Stress Management: Practice relaxation techniques like deep breathing, meditation, or yoga to reduce stress, which can exacerbate abdominal pain.
- Lifestyle Changes: Maintain a healthy weight, avoid smoking, and limit alcohol consumption as these factors can contribute to digestive issues.

Image: www.pinterest.com
Nursing Care Plan Of Abdominal Pain
A Call to Action for Better Understanding & Care
Abdominal pain can be a disconcerting experience, but understanding the nursing care plan can empower you to navigate it effectively. This roadmap for assessment, diagnosis, and treatment provides a comprehensive framework for addressing the issue. Remember, a collaborative approach between you and your healthcare provider is critical. Utilize this information to advocate for your well-being and ask questions to ensure you receive the appropriate care.
By taking an active role in your health and seeking professional guidance, you can manage abdominal pain and achieve a greater sense of well-being. Let this knowledge guide you towards a path of improved health and understanding.






