The heart is a vital organ, responsible for pumping blood throughout the body. When a portion of the heart muscle is deprived of oxygen due to a blockage in a coronary artery, it can lead to a heart attack, also known as an acute myocardial infarction (AMI). This life-threatening condition requires immediate medical attention and a comprehensive nursing care plan to ensure the patient’s survival and recovery.
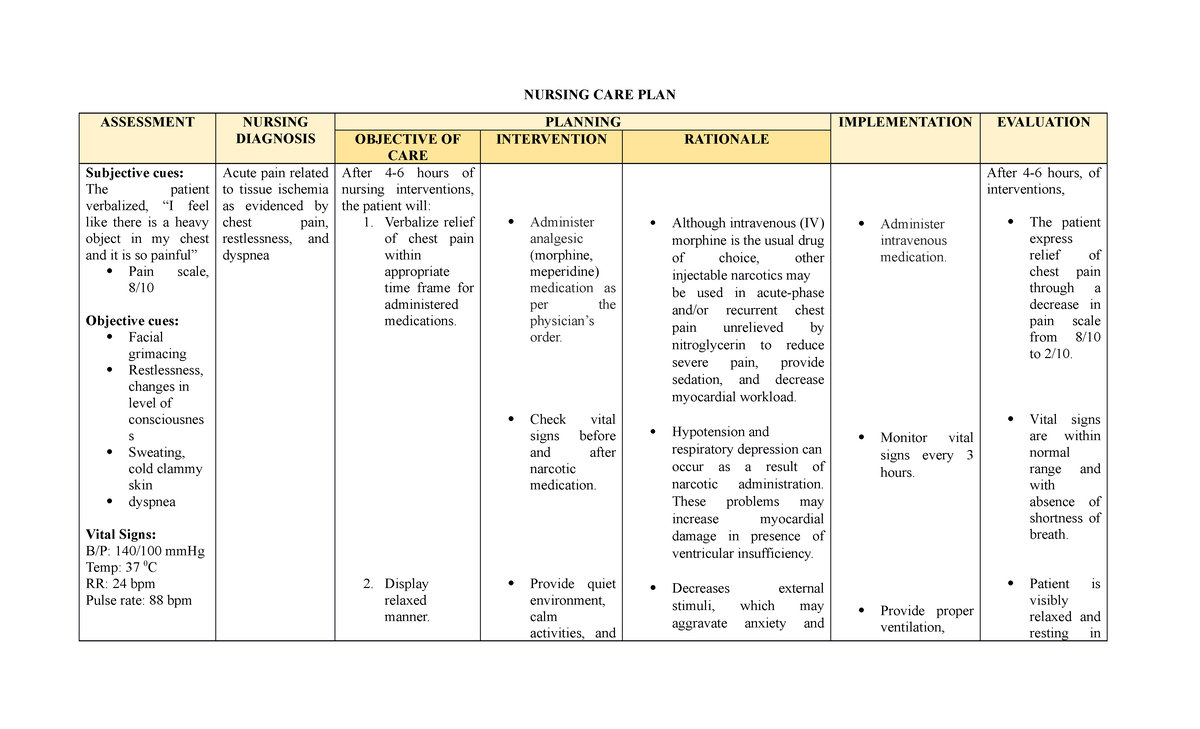
Image: www.babezdoor.com
As a nurse, I’ve witnessed firsthand the impact of AMI on patients and their families. The sudden onset of chest pain, shortness of breath, and anxiety can be overwhelming. But with a well-defined nursing care plan, we can provide the best possible care to alleviate suffering and promote healing. This article will delve into the complexities of AMI, outlining the essential elements of a nursing care plan and offering valuable insights for optimal patient management.
Understanding Acute Myocardial Infarction
Definition and Pathophysiology
Acute myocardial infarction (AMI) is a condition where a portion of the heart muscle is damaged due to a lack of oxygen. This occurs when a coronary artery, which supplies blood to the heart, becomes blocked by a blood clot. The blockage prevents blood flow to the affected area, leading to cell death. The size and location of the infarction determine the severity of the heart damage and the patient’s prognosis.
Causes and Risk Factors
The primary cause of AMI is coronary artery disease (CAD), which is characterized by the buildup of plaque in the arteries. This plaque can rupture, triggering a blood clot that blocks the artery. Risk factors for AMI include:
- High blood pressure
- High cholesterol
- Smoking
- Diabetes
- Family history of heart disease
- Obesity
- Sedentary lifestyle

Image: www.scribd.com
Signs and Symptoms
The most common symptom of AMI is chest pain, which is often described as a crushing, squeezing, or tight feeling. The pain may radiate to the jaw, neck, arms, or back. Other common symptoms include:
- Shortness of breath
- Nausea and vomiting
- Lightheadedness or dizziness
- Cold sweats
- Weakness
- Fatigue
It’s important to note that not all patients experience these classic symptoms. Some may have atypical symptoms like indigestion, jaw pain, or fatigue. In women, symptoms might include shortness of breath, nausea, or back pain. Prompt recognition and treatment are crucial for a favorable outcome.
Essential Components of an Acute Myocardial Infarction Nursing Care Plan
A comprehensive nursing care plan for patients experiencing AMI focuses on minimizing damage to the heart muscle, relieving symptoms, and preventing complications. Key components include:
1. Assessment and Early Intervention
Nurses play a vital role in assessing the patient’s condition, identifying potential complications, and initiating appropriate interventions. Key aspects include:
- Vital sign monitoring (heart rate, blood pressure, respiratory rate, temperature) to detect changes in hemodynamic status
- Electrocardiogram (ECG) monitoring for detecting cardiac arrhythmias and evidence of infarction
- Pain assessment using a standardized pain scale, to guide pain management strategies
- Assessment of neurological function for signs of stroke or other neurological complications
- Administration of oxygen to improve oxygenation and reduce myocardial workload
- Immediate initiation of cardiac medications, such as aspirin, nitroglycerin, and beta-blockers, to restore blood flow and reduce myocardial damage
2. Pain Management
Chest pain associated with AMI can be excruciating. Pain relief is a priority in nursing care. Nurses closely monitor pain levels, administer prescribed analgesics, and implement non-pharmacological interventions to enhance comfort. This may include:
- Analgesics, such as morphine or fentanyl, to reduce pain perception
- Positioning the patient to minimize strain on the chest
- Relaxation techniques, such as deep breathing exercises or guided imagery
3. Monitoring and Management of Complications
AMI can lead to a range of complications, including:
- Arrhythmias: Irregular heartbeats that can cause unstable blood pressure or fainting
- Heart Failure: The heart may be weakened and unable to pump effectively
- Cardiogenic Shock: A life-threatening condition where the heart cannot pump enough blood to meet the body’s needs
- Pericarditis: Inflammation of the sac surrounding the heart
- Thromboembolism: Blood clots that can travel to the lungs or brain
Nurses continuously monitor for these complications and implement appropriate interventions to prevent or manage them effectively. This may involve monitoring vital signs, ECG rhythms, and laboratory values, as well as administering medications and providing supportive care.
4. Education and Discharge Planning
Patient education is an integral part of the care plan. Nurses provide clear explanations about the condition, treatment strategies, and recovery process. They also emphasize the importance of adherence to medications, lifestyle modifications, and follow-up appointments.
Discharge planning begins during the hospital stay. Nurses collaborate with the patient, family, and healthcare team to develop a comprehensive plan that includes:
- Medication regimen
- Home-based cardiac rehabilitation program
- Follow-up appointments with healthcare providers
- Lifestyle changes, such as quitting smoking, managing stress, and maintaining a healthy weight
Latest Trends and Developments
The field of cardiology is rapidly evolving, bringing advancements in diagnosis, treatment, and management of AMI. Key trends include:
- Minimally Invasive Procedures: Percutaneous coronary intervention (PCI) is becoming increasingly popular. It involves threading a catheter with a balloon or stent into the blocked coronary artery, opening up the blockage and restoring blood flow.
- Telemedicine: Remote monitoring and teleconsultations allow for early detection of AMI, timely intervention, and improved patient management.
- Personalized Medicine: Genomics and bioinformatics are being integrated to tailor treatment plans based on individual genetic factors and risk profiles.
- Cardiac Rehabilitation: Comprehensive rehabilitation programs play a vital role in improving cardiac function, reducing risk factors, and promoting long-term recovery.
Tips and Expert Advice
Here are some tips for nurses providing care for patients with AMI:
- Prioritize effective communication: Clearly explain the patient’s condition and treatment plan, ensuring they understand what is happening. Empathetic communication builds trust and reduces anxiety.
- Assess and manage pain promptly: Pain management is critical, not only for comfort but also because uncontrolled pain can worsen cardiac function and increase the risk of complications.
- Be vigilant in monitoring for complications: Regularly assess vital signs, ECG rhythms, and laboratory values to identify early warning signs of complications and initiate timely interventions.
- Encourage active patient participation: Empower patients to actively participate in their care by asking questions, expressing their concerns, and actively engaging in their recovery process.
- Promote lifestyle modifications: Educate patients on the importance of lifestyle changes, such as quitting smoking, maintaining a healthy weight, and managing stress, to prevent future heart events.
Remember, consistent and compassionate care, coupled with prompt interventions, can significantly improve outcomes for patients with AMI. By staying abreast of the latest advancements in cardiac care and embracing a patient-centered approach, nurses can make a real difference in the lives of their patients.
Frequently Asked Questions
Q: What are the warning signs of a heart attack?
A: The most common symptom is chest pain, which can feel like pressure, squeezing, tightness, or pain that radiates to the jaw, neck, arms, or back. Other symptoms include shortness of breath, nausea, vomiting, lightheadedness, cold sweats, weakness, or fatigue. Not everyone experiences classic symptoms. It’s crucial to seek medical attention immediately if you suspect a heart attack.
Q: What is the role of aspirin in treating a heart attack?
A: Aspirin is crucial for treating AMI because it prevents blood clots from forming and worsening the blockage in coronary arteries. It should be administered as soon as possible to reduce myocardial damage and improve outcomes.
Q: What happens after a heart attack?
A: After a heart attack, hospitalization is usually required for monitoring and treatment. Patients typically undergo cardiac catheterization, which involves inserting a catheter into the heart to visualize the arteries. Treatment options include medications, angioplasty, or bypass surgery. Following discharge, patients need to make significant lifestyle changes and participate in cardiac rehabilitation to prevent future heart events.
Q: Can stress cause a heart attack?
A: While stress alone may not cause a heart attack, prolonged exposure to chronic stress can contribute to heart disease and increase the risk of heart events. Managing stress through relaxation techniques, exercise, and healthy coping mechanisms is crucial for cardiovascular health.
Acute Myocardial Infarction Nursing Care Plan
https://youtube.com/watch?v=r2yF76SJHbQ
Conclusion
Acute myocardial infarction is a serious medical condition requiring immediate attention and comprehensive nursing care. By understanding the pathophysiology, implementing a well-defined care plan, and staying informed about the latest advancements, nurses can provide exceptional care to patients experiencing this life-threatening event. This article has highlighted the key elements of an AMI nursing care plan, emphasizing the importance of assessment, pain management, complication monitoring, education, and discharge planning. Remember, every patient is unique, and it’s essential to tailor the care plan to meet their specific needs and challenges. Are you interested in learning more about AMI or other cardiovascular conditions? Let me know in the comments below!






