Imagine a man struggling to urinate, his bladder feeling perpetually full despite frequent trips to the restroom. This is a common reality for many men suffering from benign prostatic hyperplasia (BPH), a condition in which the prostate gland enlarges, putting pressure on the urethra and hampering the flow of urine. As a nurse, understanding the intricacies of BPH and crafting a well-defined care plan becomes paramount in ensuring the patient’s comfort and overall well-being.
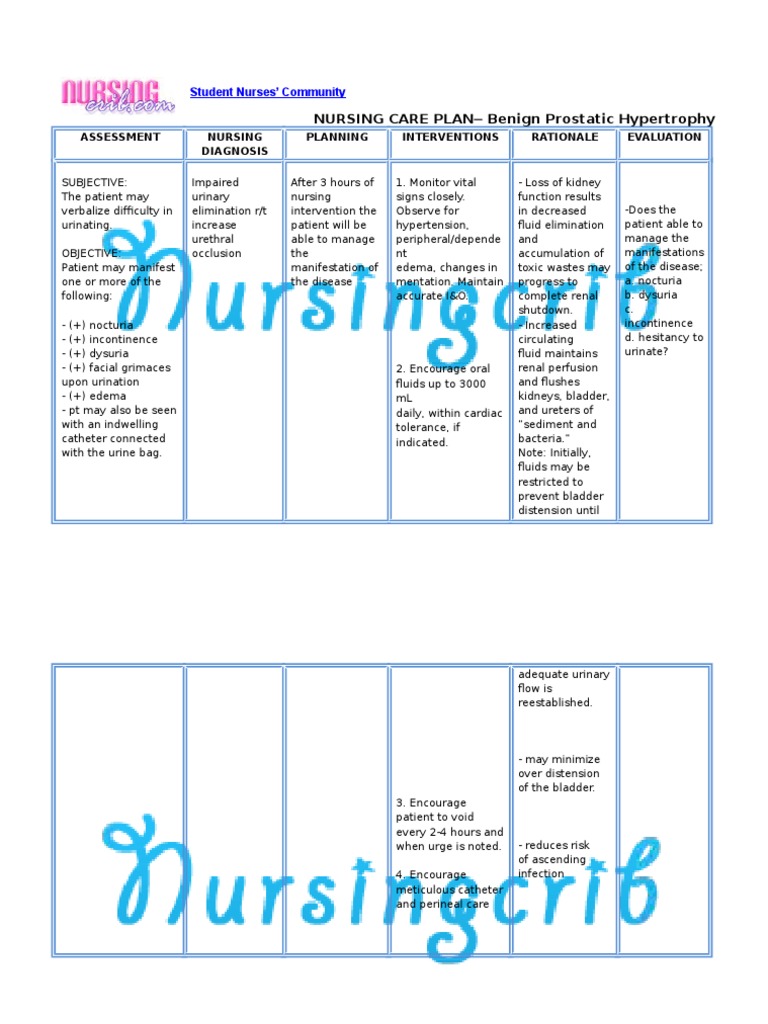
Image: www.scribd.com
This article delves into the world of benign prostatic hyperplasia, offering a detailed nursing care plan to effectively address the condition. We’ll explore the underlying causes, symptoms, and treatment options, providing a comprehensive understanding of the challenges faced by BPH patients, and how nurses can play a crucial role in their care.
Understanding Benign Prostatic Hyperplasia
What is Benign Prostatic Hyperplasia?
Benign prostatic hyperplasia (BPH), also known as prostate gland enlargement, is a common condition affecting men, particularly those over the age of 50. It’s not cancer, but rather a noncancerous growth of the prostate gland, which surrounds the urethra – the tube that carries urine from the bladder. This enlargement can put pressure on the urethra, obstructing urine flow and leading to various urinary symptoms.
Causes of Benign Prostatic Hyperplasia
The exact cause of BPH remains unknown, but it’s believed to be linked to hormonal changes as men age. As men age, their testosterone levels decline, while the dihydrotestosterone (DHT) hormone, which contributes to prostate growth, remains relatively stable. This hormone imbalance may prompt prostate cell proliferation, leading to enlargement. The exact mechanism of this process is still under investigation.

Image: www.studypool.com
Symptoms of Benign Prostatic Hyperplasia
BPH symptoms vary in severity and can range from mild inconvenience to significantly impacting quality of life. Common symptoms include:
- Frequent urination, especially at night (nocturia)
- Difficulty starting urination (hesitancy)
- Weak urine stream
- Dribbling after urination
- Feeling of incomplete bladder emptying
- Sudden urge to urinate (urgency)
- Pain or burning during urination (dysuria)
Diagnosis and Treatment
A thorough medical history, physical exam, and a digital rectal exam are usually sufficient for an initial diagnosis. Further investigations, such as a prostate-specific antigen (PSA) test and uroflowmetry, may be conducted to assess the severity of the condition. Treatment options for BPH depend on the severity of symptoms and can include:
- Watchful waiting: For mild symptoms, monitoring the condition and delaying treatment can be an option.
- Lifestyle changes: Modifying diet and exercise habits can help manage symptoms. Avoiding caffeine and alcohol, especially before bedtime, can reduce nighttime urination.
- Medications: Alpha-blockers relax muscles in the prostate and bladder neck, improving urine flow. 5-alpha reductase inhibitors reduce prostate size.
- Surgical procedures: In cases of severe BPH or complications, minimally invasive procedures like transurethral resection of the prostate (TURP) may be necessary to remove excess prostate tissue.
Nursing Care Plan for Benign Prostatic Hyperplasia
Assessment
A comprehensive assessment is the cornerstone of a successful nursing care plan. Assess the patient’s urinary symptoms, noting frequency, urgency, hesitancy, and any pain. Inquire about their lifestyle, including fluid intake, dietary habits, and smoking history. Assess their mental and emotional state, as adjusting to BPH can be stressful and may lead to anxiety or depression.
Diagnosis
Based on the assessment, formulate nursing diagnoses, focusing on the patient’s individual needs. Common nursing diagnoses include:
- Impaired urinary elimination related to prostate enlargement
- Acute pain related to urinary retention or infection
- Anxiety related to the diagnosis and impact of BPH
- Risk for urinary tract infection (UTI) related to urinary retention and obstruction
Planning
Set individualized goals based on the nursing diagnoses. For example, goals could include:
- Improved urinary elimination with decreased frequency, urgency, and hesitancy
- Relief of pain associated with BPH symptoms
- Reduced anxiety through education and support
- Prevention of urinary tract infections through hygiene and preventive measures
Interventions
Implement a variety of interventions based on the established goals. These interventions may include:
- Fluid management: Encourage adequate fluid intake and avoid fluids before bedtime to minimize nighttime urination.
- Urinary hygiene: Educate the patient about proper hygiene to prevent UTIs, including frequent handwashing and cleaning the perineal area.
- Bowel management: Constipation can exacerbate urinary symptoms. Encourage high-fiber diet and regular bowel movements.
- Medication administration: Assist with medication administration as prescribed, ensuring proper dosage and timing.
- Pain management: Provide comfort measures like warm compresses, hot baths, and analgesics to relieve pain.
- Emotional support: Offer emotional support and empathy, helping the patient cope with BPH challenges. Encourage open communication about concerns and fears.
- Education: Provide thorough education about BPH, treatment options, and self-management strategies.
Evaluation
Continuously evaluate the effectiveness of the nursing care plan. Monitor vital signs, urine output, and pain levels. Assess the patient’s emotional and mental well-being. Reassess goals and make adjustments to the plan as needed.
Tips and Expert Advice
Here are some tips for providing optimal nursing care for patients with BPH:
- Encourage open communication: Create a safe and supportive environment for patients to openly discuss their concerns, symptoms, and treatment goals.
- Promote self-management: Empower patients to manage their condition through education about lifestyle modification, medication adherence, and symptom monitoring.
- Emphasize prevention: Educate patients about potential complications of BPH, such as UTIs and urinary retention, and encourage proactive measures to prevent these issues.
- Refer appropriately: If a patient’s symptoms worsen or complications arise, ensure prompt referral to a urologist for further evaluation and treatment.
Remember that effective nursing care for BPH requires a multidisciplinary approach involving the patient, their family, and a dedicated healthcare team. By incorporating these tips into your practice, you can provide compassionate, evidence-based care and enhance the well-being of your patients with BPH.
Frequently Asked Questions
Q: What is the difference between BPH and prostate cancer?
BPH is a noncancerous enlargement of the prostate, while prostate cancer is a malignant tumor. Although both conditions can affect urination, BPH is usually more common and less serious, while prostate cancer can be life-threatening if not detected and treated early.
Q: Can BPH be cured?
While there’s no cure for BPH, it can be effectively managed through medication, lifestyle changes, or minimally invasive procedures. The goal of treatment is to improve urinary symptoms and maintain a good quality of life.
Q: Can stress worsen BPH symptoms?
While stress may not directly cause BPH, it can exacerbate existing symptoms. Stress can contribute to anxiety and sleep disturbances, which can worsen nighttime urination and other urinary symptoms associated with BPH.
Q: Are there any dietary recommendations for men with BPH?
A healthy diet rich in fruits, vegetables, and whole grains is generally recommended for overall health and may be beneficial for managing BPH. Some studies suggest that consuming foods rich in lycopene, an antioxidant found in tomatoes, may help reduce prostate size. However, further research is needed to confirm these findings.
Benign Prostatic Hyperplasia Nursing Care Plan
Conclusion
Benign prostatic hyperplasia is a common condition affecting men, and providing comprehensive nursing care is crucial for their well-being. By understanding the underlying causes, symptoms, and treatment options, nurses can effectively assess, diagnose, plan, intervene, and evaluate patient care. Open communication, patient education, and a collaborative approach are essential for managing BPH and ensuring the best possible outcomes for patients.
Are you interested in learning more about BPH nursing care or have further questions about this topic? Please share your thoughts and experiences in the comments below.






